:Carboplatin
Effects and efficacy:
Carboplatin injection is a second-generation platinum anti-tumor drug, which has certain effects on ovarian cancer, small cell lung cancer, non-small cell lung cancer, head and neck squamous cell carcinoma, esophageal cancer, testicular cancer, seminoma, bladder cancer, mesothelioma, pediatric brain tumors, etc. This product is a non-specific anti-tumor drug for the cycle, which directly acts on DNA, thereby inhibiting tumor cells with vigorous division.
Usage and dosage:
This product can be used alone or in combination with other anti-cancer drugs. Before use, add this product to 250-500ml of 5% glucose injection for dilution. For intravenous infusion, the recommended dose is calculated based on 0.3-0.4g/m2 or AUC per body surface area, a single dose, or five doses for 5 days, repeated every 3-4 weeks, and 2-4 cycles as a course of treatment. The dose after the first dose needs to be adjusted according to the white blood cell and platelet counts after the medication. Please follow the doctor's advice for details.
Adverse reactions:
Common adverse reactions Myelosuppression is a dose-related toxicity. After a single dose, white blood cells and platelets reach their lowest point 21 days after medication, and usually recover around 30 days after medication; the lowest point of granulocytes occurs 21 to 28 days after medication, and usually recovers around 35 days; white blood cell and platelet reduction is dose-related and has an accumulation effect. Pain at the injection site. Case data and post-marketing experience show that about 15% of patients experience nausea without vomiting after treatment with carboplatin, 65% experience vomiting, and 1/3 of them have severe vomiting; this product also has a certain degree of nephrotoxicity. The incidence and severity of nephrotoxicity may increase in patients with impaired renal function before treatment. Less common adverse reactions Allergic reactions (rash or itching, occasionally wheezing), which occur within a few minutes after use; peripheral neurotoxicity, numbness or tingling of fingers (toes), with cumulative effects; ototoxicity, high-frequency hearing loss occurs first, tinnitus is occasionally seen; blurred vision, mucositis or stomatitis; constipation or diarrhea, lack of appetite, etc. In addition, you may experience other side effects. If you feel unwell after taking the medicine, please inform the doctor in time. The doctor will determine whether to stop taking the medicine or take necessary measures according to the severity of the adverse reaction.
Drug contraindications:
Allergic to this product is prohibited. It is prohibited for liver and kidney dysfunction. It is prohibited to use it with caution during pregnancy and lactation.
Read more
Add to Compare
:أقراص بروكاربازين هيدروكلوريد
يعد هذا المنتج أحد الأدوية الرئيسية في بروتوكولات MOPP وCOPP القياسية لعلاج سرطان الغدد الليمفاوية الخبيثة. كما أن له تأثيرات معينة على SCLC، والورم الميلانيني الخبيث، والورم النقوي المتعدد، وأورام المخ (الابتدائية أو الثانوية)، وما إلى ذلك.
Read more
Add to Compare
Bendamustine hydrochloride ;
Bendamustine is a bifunctional alkylating agent with anti-tumor and cytocidal effects. Bendamustine, also known as bendamustine hydrochloride, is commonly used in the form of injection.
The main mechanism of the anti-tumor and cytocidal effects of this product is the cross-linking of DNA single and double strands through alkylation, which disrupts the function and synthesis of DNA, and also causes cross-linking between DNA and protein, and between protein and protein, thereby exerting an anti-tumor effect. This product is used alone or in combination with other anti-tumor drugs to treat malignant tumors such as Hodgkin's disease, non-Hodgkin's lymphoma, plasmacytoma (multiple myeloma), chronic lymphocytic leukemia (CLL), breast cancer, etc.
Read more
Add to Compare
Busulfan
Effects and efficacy:
Different dosage forms of busulfan have different indications. Busulfan tablets: used in the chronic phase of chronic myeloid leukemia, and are not effective for patients lacking the Philadelphia chromosome Ph1. It can also be used to treat chronic myeloproliferative diseases such as essential thrombocythemia and polycythemia vera. Busulfan injection: used in combination with cyclophosphamide as a pretreatment regimen before allogeneic hematopoietic progenitor cell transplantation for chronic myeloid leukemia.
Usage and dosage:
Common dosage of busulfan tablets for adults: chronic myeloid leukemia, total daily amount 4-6 mg/m2, once a day. If the white blood cell count drops to 20×109/L, the drug should be discontinued as appropriate. Or give a maintenance dose of 1-2 mg daily or every other day to maintain the white blood cell count at around 10×109/L. Busulfan injection should be administered through a central venous catheter, and each dose requires an infusion of 2 hours, once every 6 hours for 4 consecutive days, for a total of 16 times. Cyclophosphamide was given 60 mg/kg intravenously over 1 hour once a day for 2 days 3 days before bone marrow transplantation, 6 hours after the 16th dose of this product. All patients should be given phenytoin prophylactically because busulfan is known to cross the blood-brain barrier and induce epilepsy. Phenytoin reduces the plasma AUC of busulfan by 15%; other anticonvulsants may increase the plasma AUC of busulfan, thereby increasing the risk of hepatic veno-occlusive disease or epilepsy. If other anticonvulsants must be used, plasma busulfan exposure should be monitored. Antiemetics should be given before the first start and continued throughout the medication period according to a certain plan. The clearance of this product is most predictable when it is administered according to calibrated ideal body weight. If the dose of this product is calculated based on actual body weight, ideal body weight or other factors, it may result in significant differences in clearance between lean, normal and obese patients. When forming a pretreatment regimen for bone marrow or peripheral blood progenitor cell transplantation, the adult dose of this product is usually 0.8 mg/kg, taking the lower value of ideal body weight or actual body weight, and administering it once every 6 hours for 4 consecutive days (a total of 16 times). For obese or extremely obese patients, this product should be administered according to the calibrated ideal body weight. The calculation formula for ideal body weight (IBW) is as follows (height cm, weight kg): IBW (kg, male) = 50 + 0.91 (height cm-152), IBW (kg, female) = 45 + 0.91 (height cm-152). The calibrated ideal body weight (AIBW) formula is: AIBW = IBW + 0.25 (actual body weight - IBW).
Adverse reactions:
Busulfan tablets can produce bone marrow suppression. Common symptoms are granulocytopenia and thrombocytopenia. Severe cases require timely discontinuation of the drug. Long-term use or excessive use of the drug can cause pulmonary fibrosis. There may be skin pigmentation, hyperuricemia and sexual dysfunction, feminization of male breasts, testicular atrophy, and irregular menstruation in women. Cataracts, erythema multiforme rash, and polyarteritis nodosa are rare adverse reactions. There have been individual reports of epileptic seizures after high doses; endocardial fibrosis, and the corresponding symptoms; and rare hepatic venous atresia. The following section of busulfan injection describes clinically significant adverse events in clinical trials of this product, regardless of whether they are caused by the drug. Hematological system: Under the recommended dosage regimen, this product causes 100% of patients to have deep bone marrow suppression, severe agranulocytosis, thrombocytopenia, anemia, etc., so blood counts must be monitored during treatment until recovery. Gastrointestinal tract: Gastrointestinal toxicity is very common and is generally considered to be drug-related. Only a few are classified as severe toxicity. In allogeneic transplant clinical trials, 92% of patients experienced mild or moderate nausea, 95% of patients experienced mild or moderate vomiting, and 7% experienced severe nausea by 28 days after transplantation. In allogeneic transplant clinical trials, the incidence of vomiting during the administration of this product (7 days before transplantation to 4 days before transplantation) was 43%. Grade 3-4 stomatitis occurred in 26% of patients and grade 3 esophagitis in 2%. Grade 3-4 diarrhea occurred in 5% of patients in the allogeneic trial, and mild to moderate diarrhea occurred in 75%. Mild to moderate constipation occurred in 38% of patients, and ileus occurred in 8% of patients and was severe in 2%. Mild to moderate dyspepsia was reported in 44% of patients. Hematemesis occurred in 2% of patients. Pancreatitis occurred in 2% of patients. Mild to moderate rectal discomfort was seen in 24% of patients. Severe anorexia was seen in 21% of patients and mild to moderate in 64% of patients. Liver: Hyperbilirubinemia occurred in 49% of patients in the allogeneic stem cell transplantation trial. Grade 3 or 4 hyperbilirubinemia occurred in 30% of patients within 28 days of transplantation, of which 5% were life-threatening. Hyperbilirubinemia was associated with graft-versus-host disease in 6 patients and with hepatic veno-occlusive disease in 5 patients. Grade 3/4 elevations of SGPT were seen in 7% of patients. Mild to moderate elevations in alkaline phosphatase were seen in 15% of patients. Mild to moderate jaundice occurred in 12% of patients, and hepatomegaly occurred in 6%. Hepatic veno-occlusive disease: Hepatic veno-occlusive disease (HVOD) is a potential complication of pre-transplant conditioning. Graft-versus-host disease: In allogeneic studies, graft-versus-host disease (GVHD) occurred in 18% of patients; 3% were severe, 15% were mild to moderate, and severe cases could be life-threatening. Edema: 79% of patients experienced some form of edema, hypervolemia, or weight gain; all events were reported as mild to moderate. Infection/fever: 51% of patients experienced 1 or more infections. One patient had fatal pneumonia, while pneumonia was life-threatening in 3% of patients. Fever occurred in 80% of patients, 78% were mild to moderate, and 3% were severe. Chills were experienced in 46% of patients. Cardiovascular system: Mild to moderate tachycardia was reported in 44% of patients. Seven patients (11%) first reported it during administration of this product. Other arrhythmias were mild to moderate and included arrhythmias (5%), atrial fibrillation (2%), ventricular premature beats (2%), and third-degree block (2%). Mild or moderate thrombosis occurred in 33% of patients, all of which were related to central venous catheters. Hypertension was reported in 36% of patients, including grade 3/4 in 7%. Hypotension was reported in 11% of patients, grade 3/4 in 3%. Mild vasodilation (flushing or hot spots) was reported in 25% of patients. Other cardiovascular events included myocardial hypertrophy (5%), mild electrocardiographic abnormalities (2%), grade 3/4 left heart failure (1 patient, 2%), and moderate pericardial effusion (2%). Most of these events were reported after the use of cyclophosphamide. Pulmonary: Mild or moderate dyspnea occurred in 25% of patients and severe dyspnea in 2%. Severe hyperventilation occurred in 1 patient (2%); the other 2 patients (3%) were mild to moderate. Mild rhinitis and mild to moderate cough were reported by 44% and 28% of patients, respectively. Mild epistaxis was reported by 25% of patients. In the allogeneic study, 3 patients (5%) were confirmed to have alveolar hemorrhage, all of whom required mechanical ventilation support and eventually died; another patient was found to have nonspecific pulmonary interstitial fibrosis by electronic thoracoscopic wedge biopsy and died of respiratory failure 98 days after transplantation. Other pulmonary adverse events were mild or moderate, including pharyngitis (18%), hiccups (18%), asthma (8%), atelectasis (2%), pleural effusion (3%), hypoxemia (2%), hemoptysis (3%) and sinusitis (3%). Nervous system: The most reported adverse events of the central nervous system were insomnia (84%), anxiety (75%), dizziness (30%) and depression (23%); except for 1 patient (1%) who had severe insomnia, the above adverse reactions were mild or moderate. One patient (1%) experienced life-threatening cerebral hemorrhage and coma in the end-stage of multi-organ failure secondary to HVOD. Other severe adverse events included: delirium (2%), agitation (2%), and encephalopathy (2%). The overall incidence of delirium was 11%, and 5% of patients reported hallucinations. In patients who experienced delirium and hallucinations in the allogeneic studies, their delirium occurred at the completion of tadalafil dosing. In the allogeneic clinical studies of tadalafil, the overall incidence of sleepiness was 7%, and the incidence of somnolence was 2%. In the autotransplantation study, despite the administration of phenytoin prophylaxis, 1 patient still had a seizure during cyclophosphamide administration. Renal: 21% of patients had mild to moderate increases in serum creatinine. 3% of patients had increased blood urea nitrogen (BUN), and 2% of patients had grade 3/4 increases. 7% of patients had dysuria, 15% had oliguria, and 8% had hematuria. In the allogeneic clinical trials, there were 4 cases (7%) of grade 3/4 hemorrhagic cystitis. Skin: Rash (57%) and pruritus (28%) were reported, with the majority of both events being mild. Mild alopecia was reported in 15% of patients and moderate in 2%. Mild herpes was reported in 10% of patients and mild to moderate maculopapular rash in 8%. Bullae were reported in 10% of patients and exfoliative dermatitis in 5%. Erythematous nodules were reported in 2% of patients, acne in 7%, and skin depigmentation in 8%. Metabolic: Hyperglycemia was reported in 67% of patients and Grade 3/4 hyperglycemia in 15%. Mild to moderate hypomagnesemia was reported in 77% of patients; mild to moderate hypokalemia in 62% and severe hypokalemia in 2%; mild to moderate hypocalcemia in 46% and severe hypocalcemia in 3%, mild to moderate hypophosphatemia in 17%, and hyponatremia in 2%. Death: In the allogeneic transplant study, 2 deaths occurred within 28 days after transplantation; an additional 6 deaths occurred between 29 days and 100 days after transplantation. Adverse reactions of dimethylacetamide (DMA): DMA is the solvent in the formula of this product. It may cause adverse reactions such as liver toxicity (manifested as increased transaminase SGOT) and nervous system toxicity (manifested as hallucinations). Hallucinations often occur one day after the completion of the DMA dosing plan and are accompanied by EEG changes. Other neurotoxicities include drowsiness, sleepiness, and mental confusion. However, it is difficult to determine the relative extent of the effects of DMA and/or other concomitant medications in the liver toxicity and neurotoxicity observed in the use of this product. Others: Other adverse events reported included headache (mild to moderate 46%, severe 5%), abdominal pain (mild to moderate 69%, severe 3%), asthenia (mild to moderate 49%, severe 2%), nonspecific pain (mild to moderate 43%, severe 2%), allergic reaction (mild to moderate 24%, severe 2%), injection site inflammation (mild to moderate 25%), injection site pain (mild to moderate 15%), chest pain (mild to moderate 26%), back pain (mild to moderate 23%), muscle pain (mild to moderate 16%), joint pain (mild to moderate 13%) and hearing impairment (3%).
Contraindications:
Contraindicated if allergic to this product, contraindicated during pregnancy, contraindicated during lactation
Read more
Add to Compare
Chlorambucil tablets
Function and indication: This product is used for cancerous pleural and abdominal effusions; malignant lymphoma, lung cancer, seminoma, multiple myeloma, nasopharyngeal carcinoma and esophageal cancer.
Usage and dosage: The dosage and dosage of different dosage forms and specifications of this product may vary. Please read the specific drug instructions for use, or follow the doctor's advice. Nitrocarbone for injection: 20-40 mg each time, add 0.9% sodium chloride injection or 5% glucose injection 40 ml intravenous injection, or add 5% glucose injection intravenous drip, 1-2 times a week, for 2 consecutive weeks, and rest for 1-2 weeks as a cycle. Thoracic and abdominal injection, 40-60 mg each time, add 0.9% sodium chloride injection 30 ml, once a week, adjust the treatment cycle according to blood count, liver and kidney function and condition.
Adverse reactions:
1. Gastrointestinal reactions: lack of appetite, nausea, vomiting. 2. Bone marrow suppression, hair loss, fatigue. Occasionally thrombophlebitis.
Read more
Add to Compare
Cisplatin Injection.
Effects and efficacy:
Cisplatin is generally used to treat small cell and non-small cell lung cancer, testicular cancer, ovarian cancer, cervical cancer, endometrial cancer, prostate cancer, bladder cancer, melanoma, sarcoma, head and neck tumors, various squamous cell carcinomas and malignant lymphomas.
Usage and dosage:
Cisplatin can only be administered intravenously, intraarterially or intracavitary. It is usually administered by intravenous drip. Adequate hydration therapy is required 2 to 16 hours before administration and at least 6 hours after administration. Cisplatin needs to be diluted with normal saline or 5% glucose solution and then dripped intravenously. The dosage depends on the chemotherapy effect and individual response. The following dosage is for reference (for adults and children): The course of treatment depends on the clinical efficacy and is repeated every 3-4 weeks. Cisplatin can be used in combination with other anticancer drugs or alone. When used in combination, the dosage needs to be adjusted appropriately with the course of treatment.
Adverse reactions:
Nephrotoxicity After a single medium or high dose of medication, mild, reversible renal dysfunction may occasionally occur, and trace hematuria may occur. Repeated high-dose and short-term repeated use of the drug can cause irreversible renal dysfunction. In severe cases, renal tubular necrosis can lead to anuria and uremia. Digestive system symptoms include nausea, vomiting, loss of appetite, and diarrhea. The reactions usually occur within 1 to 6 hours after administration, and the longest does not exceed 24 to 48 hours. Occasionally, liver dysfunction and increased serum transaminases can be seen, which can be restored after drug withdrawal. The hematopoietic system is manifested by a decrease in white blood cells and (or) platelets, which is generally related to the dosage of the drug. Bone marrow suppression generally reaches a peak in about 3 weeks and recovers in 4 to 6 weeks. Ototoxicity can cause tinnitus and high-frequency hearing loss, which are mostly reversible and do not require special treatment. Neurotoxicity is more common in patients with a total amount of more than 300 mg/m2. Peripheral nerve damage is common, manifested as ataxia, myalgia, and paresthesia of the upper and lower limbs. A small number of patients may experience brain dysfunction, and epilepsy and retrobulbar neuritis may also occur. Allergic reactions such as increased heart rate, decreased blood pressure, dyspnea, facial edema, and allergic fever reactions may all occur. Other hyperuricemia: Leg swelling and joint pain are common. Plasma electrolyte disorders: hypomagnesemia, hypocalcemia, muscle cramps. Cardiac toxicity: Rare arrhythmias, electrocardiogram changes, bradycardia or tachycardia, heart failure, etc. Immune system: Immunosuppressive reactions may occur. Gingival changes: Platinum metal deposits may appear on the gums. Patients may experience local swelling of the limbs where arterial or intravenous injections are given. Pain, erythema and skin ulcers, local phlebitis, etc. are rare. Hair loss, sperm and egg formation disorders, and male breast feminization may also occur. The occurrence of secondary non-lymphocytic leukemia is related to the use of cisplatin chemotherapy. Vascular lesions, such as cerebral ischemia, coronary artery ischemia, peripheral vascular disorders similar to Ravnaud syndrome, and other side effects are rare, but may be related to the use of cisplatin.
Drug contraindications:
Contraindicated during lactation, contraindicated during pregnancy, and contraindicated for allergies to this product
Read more
Add to Compare
Darolutamide Tablets.
Darolutamide Tablets.Daroltamide tablets are a Western medicine. They are clinically used to treat adult patients with non-metastatic castration-resistant prostate cancer (NM-CRPC) who have a high risk of metastasis.
The main ingredient of Daroltamide tablets is daroltamide, an androgen receptor (AR) inhibitor that competitively inhibits the binding of androgens to AR, thereby inhibiting AR nuclear translocation and AR-mediated transcription.
Read more
Add to Compare
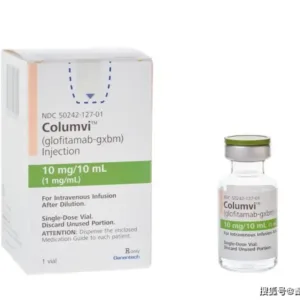
Glofitamab Injection.
How effective is glofitamab in treatment? Glofitamab (glofitamab-gxbm) is a bispecific antibody that can simultaneously target CD3 and CD20, activating T cells to release cancer cell-killing proteins. Clinical trials have shown that it has significant efficacy in treating relapsed or refractory diffuse large B-cell lymphoma, with a complete remission rate of 40% and an objective remission rate of 52%. The drug performed well in clinical trials, with significant efficacy and high safety, greatly improving the quality of life of patients.
Diffuse large B-cell lymphoma and follicular lymphoma are common malignant tumors that have a serious impact on the lives of patients. In recent years, glofitamab (glofitamab-gxbm), as a new monoclonal antibody drug, has shown good efficacy in the treatment of relapsed or refractory diffuse large B-cell lymphoma and large B-cell lymphoma caused by follicular lymphoma. This article will specifically discuss the therapeutic efficacy of glofitamab.
1. The therapeutic mechanism of Gefituzumab
Gefituzumab is a bispecific antibody that achieves targeted killing of cancer cells by binding to two proteins, CD20 and CD3. CD20 is a leukocyte antigen widely expressed on the surface of B-cell malignant tumor cells, while CD3 is a membrane protein on the T-cell receptor that participates in cellular immune responses. When Gefituzumab binds to CD20 and CD3, they activate T cells and cause them to attack and kill cancer cells. This new immunotherapy can effectively promote the clearance of tumor cells by the immune system.
2. Clinical trial results of Gefituzumab
Recent studies have shown that Gefituzumab has shown significant efficacy in the treatment of relapsed or refractory diffuse large B-cell lymphoma and large B-cell lymphoma caused by follicular lymphoma. Clinical trial data show that the drug has produced a high overall response rate and complete remission rate in patients with these malignant tumors. After receiving Gefituzumab treatment, many patients have significantly reduced tumor size, relieved symptoms, and prolonged survival.
3. Advantages and safety of Gefituzumab
Compared with traditional chemotherapy and other immunotherapies, Gefituzumab has unique advantages. First, due to its specific binding mechanism, Gefituzumab can more accurately identify malignant tumor cells and reduce damage to normal cells, thereby reducing adverse reactions during treatment. Secondly, Gefituzumab uses bispecific antibody technology, which can more effectively activate T cells and enhance immune killing effects. In addition, the medication regimen of Gefituzumab is also more convenient, allowing patients to have a more effective and comfortable treatment experience.
Regarding the safety of Gefituzumab, current clinical data show that it is well tolerated in most patients. Common adverse reactions include fever, respiratory tract infection, fatigue, etc., but most reactions are mild or moderate and can be alleviated by appropriate supportive treatment. In clinical use, patients' drug reactions and adverse events still need to be closely monitored to ensure the safety and effectiveness of treatment.
4. Further research and application prospects of Gefituzumab
Although Gefituzumab has shown potential in the treatment of large B-cell lymphoma, its therapeutic effect in different types of malignant tumors and other diseases still needs further research and verification. With the development of science and technology and a deeper understanding of tumor biology, we can expect Gefituzumab and its similar drugs to play a wider role in tumor treatment in the future.
As a new type of immunotherapy drug, Gefituzumab has shown good efficacy in the treatment of relapsed or refractory diffuse large B-cell lymphoma and large B-cell lymphoma caused by follicular lymphoma. Its targeted effect and good tolerability make it a promising treatment option, providing patients with new survival opportunities and the possibility of improving their quality of life. With further research, we can expect more applications of Gefituzumab in tumor treatment.
Read more
Add to Compare
Ibrutinib Capsules.
Ibrutinib capsules are a related drug for the treatment of blood lymphomas. The main indications are:
This product is suitable for the treatment of patients with mantle cell lymphoma who have received at least one previous treatment.
This product is suitable for the treatment of patients with chronic lymphocytic leukemia/small lymphocytic lymphoma.
This product is suitable for the treatment of patients with Waldenstrom's macroglobulinemia who have received at least one previous treatment, or the first-line treatment of patients with Waldenstrom's macroglobulinemia who are not suitable for chemoimmunotherapy.
This product is used in combination with rituximab for the treatment of patients with Waldenstrom's macroglobulinemia.
Read more
Add to Compare
Product Categories
- A الهضم والتمثيل الغذائي
- B تداول البلازما
- C نظام القلب والأوعية الدموية
- D الاستعدادات الجلدية
- DR\MR المطور المحسن
- E أدوية الجهاز المكونة للدم
- F نظام الدماغ القحفي
- G الجهاز البولي التناسلي
- H الاستعدادات الهرمونية
- K الهرمونات الجنسية
- M الجهاز العضلي الهيكلي
- N أدوية الجهاز العصبي
- O الأدوية المساعدة للأورام
- P مضادات الديدان
- R الجهاز التنفسي
- S الفم والعينين والأنف والأذنين
- Vترياق التسمم
- W الحد من البرد والحمى
- X أمراض معدية
- أدوية الأورام
- الأدوات الطبية
- الأدوية المضادة للعدوى
- السواغات الطبية
- الطعام الصحي
- منتجات الصحة الجنسية
Brands
Selected static block was removed or unpublished